Improving the odds: Researchers develop novel device to study early stage of breast cancer
Imagine your chances of developing an invasive cancer were the same as a coin toss. Do you opt for aggressive treatments like surgery and chemotherapy, or do you take your chances that the cancer will never manifest?
This is the dilemma clinicians and their patients diagnosed with DCIS, the earliest stage of breast cancer, are facing today. Ductal carcinoma in situ (DCIS) is a situation in which cancer tumor cells grow inside the mammary ducts. As long as the tumor cells remain trapped in the ducts, a patient could be fine for decades with no treatment.
But 25 to 50 percent of DCIS patients will develop an invasive cancer, the tumor cells spilling out of the mammary ducts and spreading around the body. To date, there is no reliable method to determine which patients will fall into which category.
Researchers at the Morgridge Institute for Research and the University of Wisconsin-Madison are trying to address this problem by studying the development of DCIS—and its transition to an invasive cancer—using metabolic imaging and novel microfluidic devices. The team’s latest work was recently published in the journal EBioMedicine.
Jose Ayuso, a postdoctoral fellow at Morgridge and UW-Madison and first author on the paper, says understanding how cancer cells survive in the harsh environment of the mammary ducts is one core component of the project. Inside the mammary ducts, cancer cells don’t have a blood supply, so the cells should die due to severe lack of oxygen and nutrients.
“Somehow these cancer cells can adapt to the lack of oxygen and nutrients and become very aggressive and invasive in that environment,” Ayuso says.
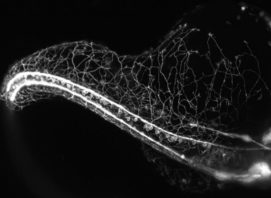
In order to study the complex process of DCIS transition to invasive cancer, the researchers developed a device that mimics the structure of the mammary duct and the density of cells within. It requires a hollow cylinder with normal cells forming the wall of the duct and tumor cells inside. It’s a specific configuration that doesn’t lend itself well to a petri dish, the common biological lab device.
“Comparing the native DCIS environment in the body with a plastic petri dish in the lab is like comparing a car in real life with a toy; it’s missing a lot of the parts,” Ayuso says. “With the microfluidic device we can better mimic the tumor microenvironment.”
In the study, cell behavior was monitored using confocal microscopy and optical metabolic imaging, and the microfluidic device proved to be a successful model of the DCIS structure and microenvironment. The researchers also showed that targeting cells capable of withstanding the harsh conditions of the mammary ducts—tumor cells that modified themselves genetically so they could survive the lack of oxygen and nutrients—could provide new avenues for therapies.
Ayuso says much of the project’s success comes down to the diverse expertise of the team. Ayuso works with collaborators like Dave Beebe, an expert in bioengineering and cancer biology in the Departments of Biomedical Engineering and Pathology and Laboratory Medicine at UW-Madison; Melissa Skala, an investigator at the Morgridge Institute with expertise in metabolic imaging of cancer; and Kari Wisinski, a clinician with the Carbone Cancer Center at UW-Madison who provides the patient and clinician perspective.
The next challenge for the team: clinical translation.
While the use of microfluidic devices and metabolic imaging proved to be useful, these methods require nontraditional tools and very specific expertise that would be difficult, if not impossible, to implement in the clinic setting.
“Using microfluidics and metabolic imaging is more complicated than a simple blood draw,” Ayuso says. “We’re working to translate our findings into a simple, user-friendly test that could be implemented in any hospital. That’s the critical next step for bringing this to the clinic.”